Sleep Hygiene and ME/CFS
– an exploration of alternatives to the standard advice -
We all know sleep is important. Sleep is how we restore and repair. But what if one of the central symptoms of your condition is unrefreshing sleep? How do you manage then?
I find unrefreshing sleep to be one of the most frustrating symptoms of ME/CFS. I can do all the ‘right’ things, follow sleep hygiene advice, get what ‘should’ be a full night of sleep and still wake up feeling like I’ve only had a few hours of sleep.
Image description: a graphic on a tan background with blue text boxes. Heading: ‘Sleep Hygiene and ME/CFS’. Sleep hygiene strategies are designed to support getting the recommended 7-9 hours of sleep a night for adults. They focus on things like bedroom environment, activity during the day, food timing, and routines around sleep. There is some inherent ableism in many sleep hygiene tips that assume ability, capacity and resources that not everyone has. They need some adaptations to be suitable for people with conditions like ME/CFS, other chronic illnesses and/or neurodivergence. And within these populations, further individualisation may be necessary to accommodate individual differences. Small images: top left is a clock wearing a hat with zzzs going up; top right is an outline of a head with a low battery image inside it; bottom left is a person slumped over their arms with red splurts above their head; bottom right a group of stick figures in different colours and positions.
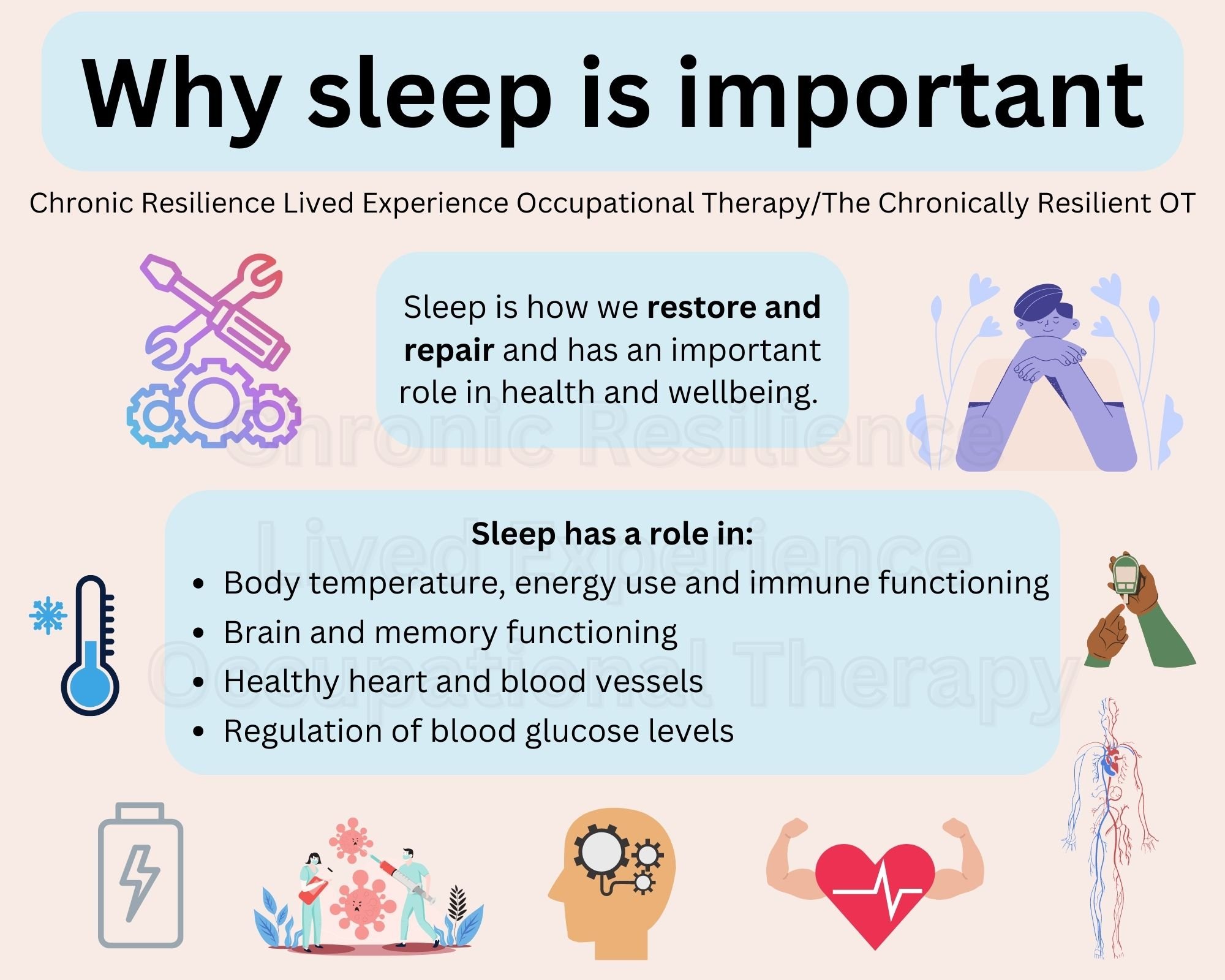
The National Sleep Foundation recommends that adults get 7-9 hours of sleep a night. Health Navigator talks about sleep’s important role in health and wellbeing. They list sleep’s role in important body processes and link lack of sleep to increased risk of developing long term health problems. Sleep has a role in:
Body temperature, energy use and immune functioning;
Brain and memory functioning;
Healthy heart and blood vessels;
Regulation of blood glucose levels.
They also list the signs of not getting enough sleep which are similar to many ME/CFS symptoms such as mood and cognitive problems, reduced activity, food cravings, lower libido, tiredness and lethargy during the day, and getting sick more often.
Image description: a graphic on a tan background with blue text boxes. Heading: ‘Why sleep is important’. Sleep is how we restore and repair and has an important role in health and wellbeing. Sleep has a role in: Body temperature, energy use and immune functioning; Brain and memory functioning; Healthy heart and blood vessels; Regulation of blood glucose levels. Images: top left 3 cogs with crossed spanner and screwdriver; top right a purple person resting their head in their hands looking relaxed with flowers on each side; across the bottom left to right: a thermostat, a battery, people fighting off germs, an outline of a head with cogs inside, a heart with muscly arms, the circulatory system, a blood glucose monitor.
—————————————
So what is sleep hygiene?
First let’s talk about circadian rhythm. This is your internal body clock that is on a 24 hour cycle and controls when you feel tired or alert. Feelings of tiredness will peak in the evening in relation to this cycle. Your circadian rhythm is also impacted by exposure to daylight and the release of the hormones melatonin and cortisol. Melatonin is released in the evening as natural light reduces and helps us to feel drowsy. Cortisol is released in the morning with the rising of sun to increase alertness. For more see https://www.sleepfoundation.org/how-sleep-works/why-do-we-need-sleep.
Sleep hygiene recommendations (or good sleep habits) often focus on supporting the circadian rhythm, as well as environmental changes, routines at bedtime and activity throughout the day. Sleep hygiene tips are designed to support getting the recommended 7-9 hours of sleep a night for adults. Most sleep hygiene tips assume ability and capacity and can come across as quite ableist. They need some adaptations to be suitable for people with conditions like ME/CFS.
Image description: a graphic on a tan background with blue text boxes. Heading: ‘Circadian rhythm.’ Your internal body clock is on a 24 hour cycle, which controls when you feel tired or alert. Feelings of tiredness will peak in the evening in relation to this cycle. Your circadian rhythm is also impacted by exposure to daylight and the release of hormones such as melatonin and cortisol. Melatonin is released in the evening as natural light reduces and helps us to feel drowsy. Cortisol is released in the morning with the rising of sun to increase alertness. Images: top left – an outline of a head with a clock and the numbers 24 inside it, on one side is a moon and on the other a sun, arrows join the sun and moon around the outside of the head to represent the 24 hour body clock; bottom right: a representation of the melatonin and cortisol cycle, cortisol rises in the morning helps us wake up and keep going, melatonin rises in the evening, helps with feeling sleepy, this is represented by wavy red and blue lines, with a moon and sun at the top to represent day and night.
I often talk about sleep hygiene strategies in relation to a 24 hour sleep cycle. Sleep hygiene strategies are not just about what we do in the hour before bed, what we do in each 24 hour period can impact how we sleep, including things like what time we wake up, how much natural light we get, when we move our bodies, rest or eat, how we wind down, when we go to sleep and what we do if we wake in the night.
Image description: a graphic on a tan background with blue text boxes. Heading: ‘The 24 hour sleep cycle.’ Sleep hygiene is not just what we do in the hour before bed, what we do throughout our day plays a role in keeping our sleep on track. In the centre is a clock with an arrow around the outside. Different coloured cloud shapes note the different factors that can impact sleep: consistent wake time; Some exposure to natural light, or a lamp that mimics natural light, during the day; Some activity through the day, balanced with rest; Food timing; Winding down routine; Consistent bed time; Bedroom environment suitable for sleep; Have a plan for what to do if you wake in the night.
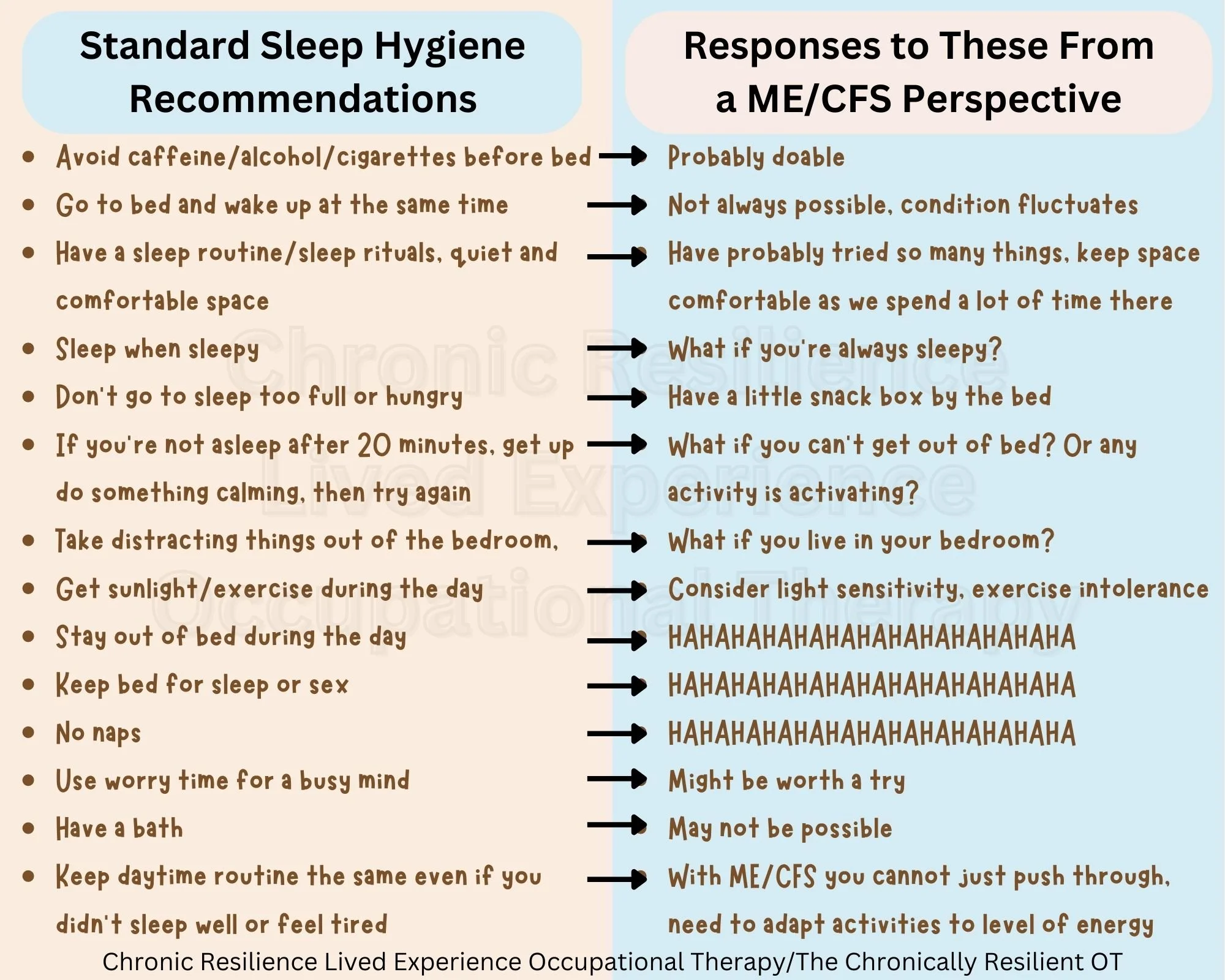
Standard sleep hygiene tips
(for the sources I used see here and here, this advice is repeated on most pages about sleep hygiene)
Regular sleep and wake times, go to bed and wake up at the same time each day, including weekend, if you are staying awake in bed for a long time in the evening you may need a later bedtime;
Your body clock is set by exposure to light – get outside or sit by a bright window for at least 30 minutes in the morning, reduce lights in the evening and turn off screens at least 30 minutes before bed (the light can interfere with melatonin levels);
Sleep when sleepy, get up and try again if you haven’t been able to get to sleep after about 20-30 minutes, do something calming or boring in another room then return to bed and try again, do not use a screen, eat or do chores, go back to bed when sleepy;
Avoid caffeine, nicotine and alcohol for at least 4-6 hours before bed, alcohol can make it harder to stay asleep;
Use bed only for sleeping or sex, to help the body associate bed with sleep and not other activities. Stay out of bed during the day and do not spend too long in bed awake;
Avoid naps, or if necessary make sure it’s less than an hour and before 3pm, naps count in the 7-9 recommended hours of sleep, if naps are making it harder to fall asleep at night try without;
Sleep rituals/routine can help remind your body it’s time for bed, develop a relaxing sleep routine for the hour before bed to help you wind down – e.g. meditation, tea, music, reading; avoid stimulating activities like exercise, computer games, TV, movies, important discussions;
Have a hot bath 1-2 hours before bedtime as the body temperature drop afterwards will help you feel sleepy;
Avoid clock-watching as this can increase worry thoughts, try not to worry about having a bad sleep, rest is still good;
Use worry time if your thoughts are keeping you awake;
Try using a sleep diary for 2 weeks to capture the facts about your sleep;
Exercise during the day to help with feeling tired at night, avoid vigorous exercise 4 hours before bed as this could keep you awake;
Food timing – avoid going to bed with a full stomach or being too hungry, big meal at least 2 hours before bed, light snack at bedtime if going to bed on an empty stomach is distracting;
Sleep environment – quiet and comfortable, cool room 16-18 degrees celcius, blankets for warmth, pillows for comfort, curtains/eye mask, earplugs if necessary, take distracting things out of the bedroom (e.g. computer, TV, radio, phone, cover clocks);
Consistency of daytime routine – keep daytime activities consistent, even if you’ve had a bad night of sleep, avoiding activities when you feel tired can reinforce insomnia;
See your GP if you’ve tried everything and sleep is not improving.
Image description: a graphic split into two sides with bullet points. On the left the heading is ‘standard sleep hygiene recommendations’ and below: Avoid caffeine/alcohol/cigarettes before bed; Go to bed and wake up at the same time; Have a sleep routine/sleep rituals, quiet and comfortable space; Sleep when sleepy; Don't go to sleep too full or hungry; If you're not asleep after 20 minutes, get up do something calming, then try again; Take distracting things out of the bedroom; Get sunlight/exercise during the day; Stay out of bed during the day; Keep bed for sleep or sex; No naps; Use worry time for a busy mind; Have a bath; Keep daytime routine the same even if you didn't sleep well or feel tired. Crossing over the divide in the middle are arrows to the right side headed ‘responses to these from a ME/CFS perspective: Probably doable; Not always possible, condition fluctuates; Have probably tried so many things, keep space comfortable as we spend a lot of time there; What if you're always sleepy?; Have a little snack box by the bed; What if you can't get out of bed? Or any activity is activating?; What if you live in your bedroom?; Consider light sensitivity, exercise intolerance; HAHAHAHAHAHAHAHAHAHAHAHAHA; HAHAHAHAHAHAHAHAHAHAHAHAHA; HAHAHAHAHAHAHAHAHAHAHAHAHA; Might be worth a try; May not be possible; With ME/CFS you cannot just push through, need to adapt activities to level of energy.
Sleep hygiene for ME/CFS
The above sleep hygiene tips for good sleep habits have been well-researched and absolutely do work for some people. However, some strategies are just not suitable and some need adjustments to make them work for an individual, especially those with ME/CFS or other conditions where unrefreshing sleep is a central feature. This is where it feels like the strength of occupational therapy comes in as we look at factors within the
Person (illness, symptoms, movement capacity, sensitivity to light etc.)
Environment (bedroom, home, supports etc.)
Occupation (sleep)
that are barriers or facilitators and go from there to problem solve solutions and strategies and figure out with the person what is going to work for them. This is likely to take some trial and error and of course any changes to habits takes time. Improving sleep habits is never a quick fix but it is something that can make a big difference to your overall health.
Resources I found online mention that sleep is important to address in ME/CFS, but most don’t go beyond the standard sleep hygiene principles. Although this resource from the Sleep Health Foundation does acknowledge that the fatigue of ME/CFS isn’t the same as sleepiness, and that the condition involves unrefreshing sleep and the need for extra rest to recover from activity. The resource notes that sleep ins and naps may be required but to be cautious about sleeping too late and going to bed late and then refers over to a standard sleep hygiene resource. So there’s something, but not much. This paper recommends sleep hygiene and relaxation strategies for managing ME/CFS symptoms but provides no further details of what this involves.
The new NICE guidelines (which have been updated to remove GET) provide recommendations on rest and sleep for people with ME/CFS (see picture).
An article by Jackson and Bruck (2012) reviewed sleep differences in people with ME/CFS noting some evidence for reduced total sleep time and sleep efficiency, increased number and duration of wakings, taking longer to get to sleep, possible differences in time spent in different sleep stages and transitions between stages, and reduced heart rate variability which can indicate that the nervous system stays alert.
This blog by Bruce Campbell from ME/CFS & Fibromyalgia Self-Help outlines three categories for sleep management plans: sleep environment and habits, medications, sleep disorders; and has some useful suggestions that would be doable by some. Dr Vallings also has a resource outlining 5 approaches for sleep management in ME/CFS: environmental, lifestyle changes, self help strategies, symptom relief and medication.
Image description: a screenshot of an extract from the NICE guildelines for ME/CFS of the section on rest and sleep. Title: Rest and sleep. 1.12.1 - Advise people with ME/CFS: about the role of rest in ME/CFS; that rest periods are part of all management strategies for ME/CFS; how to introduce rest periods into their daily routine, including how often and for how long, as appropriate for each person; that relaxation techniques at the beginning of each rest period could be helpful. 1.12.2 - Give people with ME/CFS personalised sleep management advice that includes: explaining the role and effect of sleep disturbance in ME/CFS identifying the common changes in sleep patterns seen in ME/CFS (such as broken or shallow sleep, altered sleep pattern or hypersomnia); developing good sleep habits; taking into account the need for rest in the day, and balancing this against how the person is sleeping at night; introducing changes to sleep patterns gradually. 1.12.3 - If sleep management strategies do not improve the person's sleep and rest, think about the possibility of an underlying sleep disorder or dysfunction and whether to refer to an appropriate specialist. 1.12.4 - Review the use of rest periods and sleep management strategies regularly as part of the person's care and support plan.
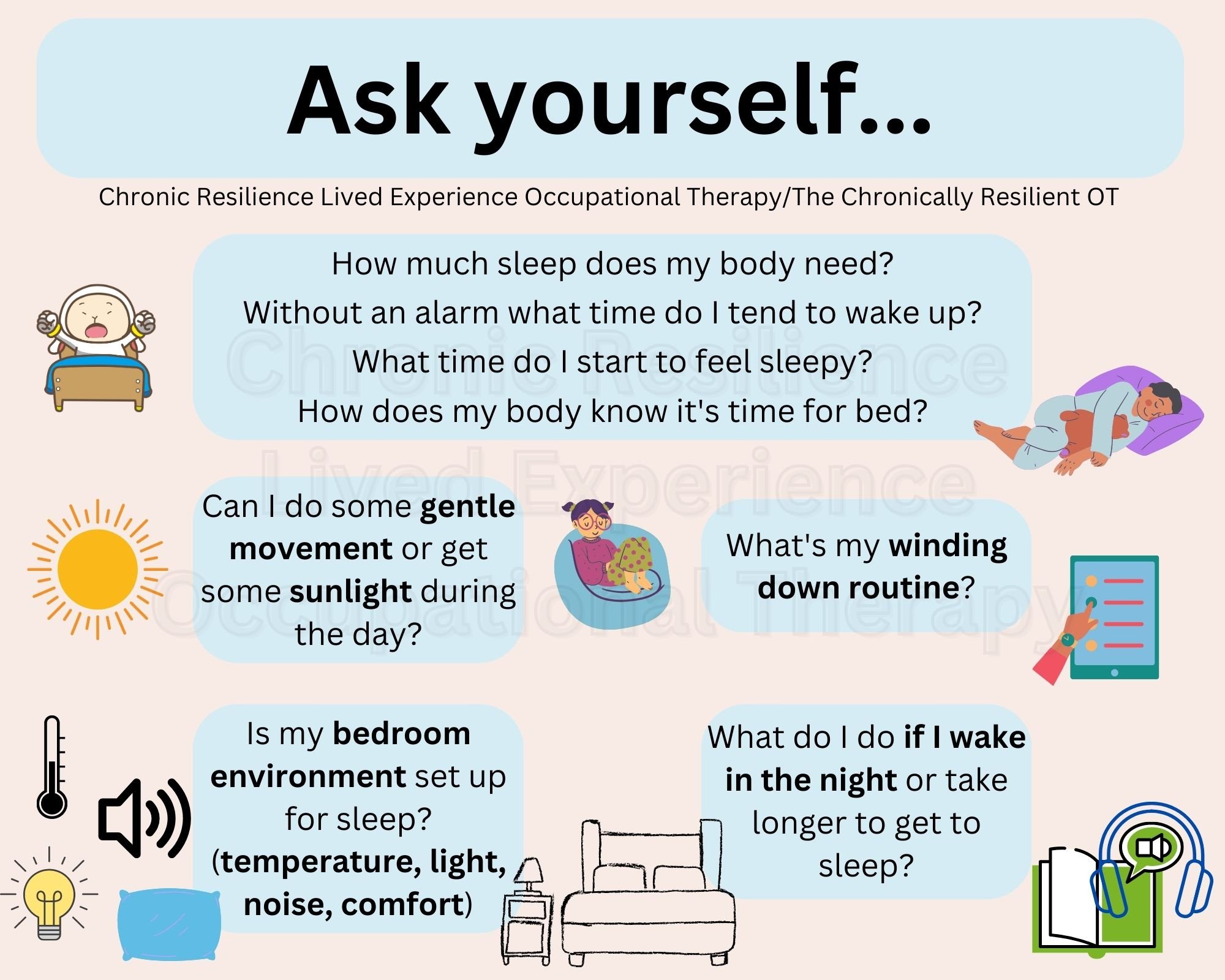
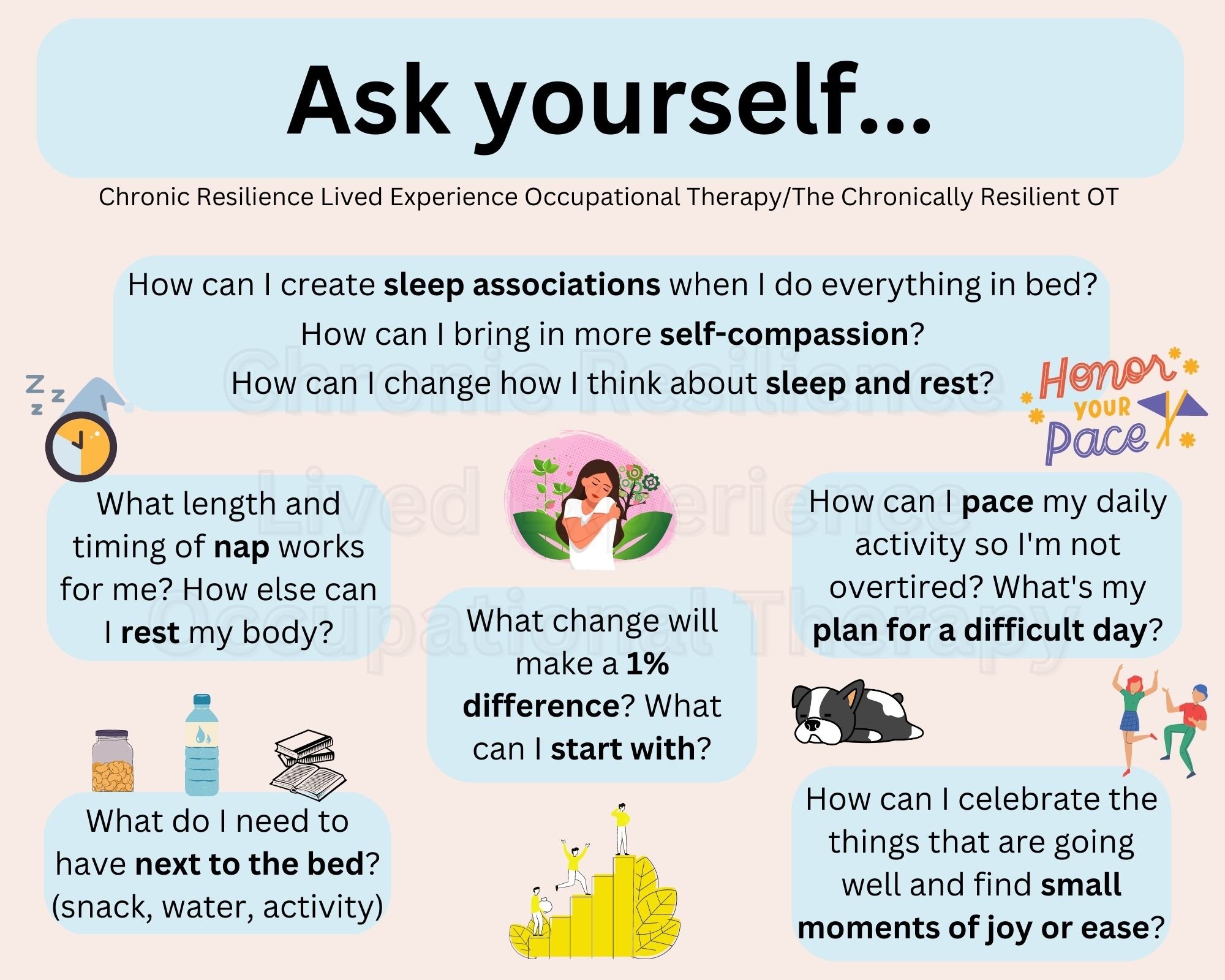
Alternatives, adaptations and questions to personalise standard sleep hygiene advice
Image description: [left] a graphic on a tan background with blue text boxes. Heading: ‘Ask yourself...’ How much sleep does my body need? Without an alarm what time do I tend to wake up? What time do I start to feel sleepy? How does my body know it's time for bed? Can I do some gentle movement or get some sunlight during the day? What’s my winding down routine? Is my bedroom environment set up for sleep? (temperature, light, noise, comfort). What do I do if I wake in the night or take longer to get to sleep? Images: a sheep waking up in bed, a person lying on a pillow with a toy cuddled into them, a sun, a person sitting on a comfy chair, a list, thermometer, sound symbol, lightbulb, pillow, bedroom, book with headphones.
Image description: [right] a graphic on a tan background with blue text boxes. Heading: ‘Ask yourself...’ How can I create sleep associations when I do everything in bed? How can I bring in more self-compassion? How can I change how I think about sleep and rest? What length and timing of nap works for me? How else can I rest my body? What change will make a 1% difference? What can I start with? How can I pace my daily activity so I'm not overtired? What's my plan for a difficult day? What do I need to have next to the bed? (snack, water, activity). How can I celebrate the things that are going well and find small moments of joy or ease? Images: clock with a hat and zzzs, person hugging themselves, a snack jar, water, bottle, books, stepping up, a sleepy dog, 2 people celebrating, ‘honour your pace’ with flags.
————————————————
So let’s go through the standard sleep hygiene advice and make suggestions of how the standard tips might be adapted, including questions you might ask yourself. Suggestions and adaptations will have to be general in nature as every person is different and has their own set of personal and environmental factors, this is to give you an idea of how things might be adapted to suit.
Regular sleep and wake times, go to bed and wake up at the same time each day, including weekends, if you are staying awake in bed for a long time in the evening you may need a later bedtime
Questions to ask: does your schedule allow for this? Are you caring for others? Do you resist structure or do well with this? Do you need as much sleep as you can get and so do sleep in? Does a rigid schedule increase anxiety if you don’t get to sleep on time? Do you need a later bedtime? How do you feel when you have a regular sleep/wake time? If you had no responsibilities or obligations what time would suit you for waking? Does your sleep/wake cycle shift during the month? This can be linked to hormones and menstrual cycles. If you have certain times of the month when you are more energised in the evening, what would it be like to just go with that instead on beating yourself up for not being able to sleep? If you have times where you need more sleep, then can you go to bed earlier or have a nap?
Ways to adapt: have a sleep window and aim to get to sleep within that window, for example bedtime between 10-11pm, wake between 8-9am; have a plan for what to do on evenings when it is harder to go to sleep and you might stay up later, use self-validation and self-compassion; have a plan for allowing sleep ins if needed; shift your bedtime to suit your sleep/wake cycle if possible; notice how your energy fluctuates over the month and whether you need to adjust your bedtime and expectations during different stages of your cycle (if you menstruate).
Your body clock is set by exposure to light – get outside or sit by a bright window for at least 30 minutes in the morning, reduce lights in the evening and turn off screens at least 30 minutes before bed (the light can interfere with melatonin levels)
Questions to ask: can you tolerate natural light or do you have a light sensitivity? Does light increase your symptoms? How could you get some light during the day? Is screen time how you wind down in the evening? Could you or do you want to change this? What lights could you reduce in the evening?
Ways to adapt: spend some time lying near a window or outside if you can, open the curtains, get a lamp that mimics sunlight, go for a short walk outside if you can; in the evening reduce ambient light, use lamps instead of bright overhead lights, use the settings on your phone or computer to make the light of your screen more yellow and less blue, there are glasses you can get that block blue light too, be aware of what you’re using a screen for and make sure it’s not too activating for your system.
Sleep when sleepy, get up and try again if you haven’t been able to get to sleep after about 20-30 minutes, do something calming or boring in another room then return to bed and try again, do not use a screen, eat or do chores, go back to bed when sleepy
Questions to ask: can you get up? Do you have another space to go to? What do you find calming or boring? How can you help yourself wind down? Are you even tired? Do you need to change your bedtime? Is falling asleep within 20-30 minutes normal for you or does it take longer?
Ways to adapt: have a few calming activities next to your bed (e.g. crosswords, colouring), play a meditation recording or audiobook, do a body scan or other mindfulness activity, notice but don’t get hung up on thoughts as stressing about not sleeping is not going to help, appreciate the rest as being useful even if it’s not sleep, remind yourself that sometimes it does take longer to fall asleep and that’s ok, if your body and mind are somewhat calm, stay in bed and the rest will still be nourishing for your body.
Avoid caffeine, nicotine and alcohol for at least 4-6 hours before bed, alcohol can make it harder to stay asleep
Questions to ask: do you use any of these? Do you notice if they have an impact on your sleep? How could you cut down or not do these 4-6 hours before bed? Does caffeine actually help you sleep (this can be the case for some ADHDers)?
Ways to adapt: if you smoke, try having fewer cigarettes in the evening; avoid caffeine in the afternoon, find the time that works for you to stop; remind yourself that alcohol can make sleep quality worse – if you’re concerned about your drinking or want to quit smoking then seek additional support; maybe caffeine helps you sleep, do what you need to do.
Use bed only for sleeping or sex, to help the body associate bed with sleep and not other activities. Stay out of bed during the day and do not spend too long in bed awake
Questions to ask: is this even feasible for you? Do you have another space to do activities and rest during the day? Is bed the best place for you to do other activities? (and it’s ok if the answer is yes)
Ways to adapt: if you are bedbound or spend a lot of time in bed, you can create sleep associations in other ways e.g. a song, recording, meditation, object, being on top of or under the blanket, brushing teeth, changing into pyjamas, eye mask – anything that works for you and reminds your body it’s bedtime; if you’re spending a lot of time in bed awake, how can you be resting your body and mind, even if it’s not sleep this rest is still useful e.g. body scans, breathing, mindfulness, stillness or gentle movement.
Avoid naps, or if necessary make sure it’s less than an hour and before 3pm, naps count in the 7-9 recommended hours of sleep, if naps are making it harder to fall asleep at night try without
Questions to ask: how much sleep do you need? How do you feel with or without naps? Does napping impact your sleep? What times during the day do you generally feel sleepy? Do you do best with short 20 minute naps or an hour or more?
Ways to adapt: if you need to nap then nap, listen to your body, work out a timing and length of nap that works for you; or if you’re not napping during the day then at least have some lying down rest time so that you’re not too overtired at bedtime; if a nap isn’t impacting your night time sleep, then you need the extra sleep.
Sleep rituals/routine can help remind your body it’s time for bed, develop a relaxing sleep routine for the hour before bed to help you wind down – e.g. meditation, tea, music, reading; avoid stimulating activities like exercise, computer games, TV, movies, important discussions
Questions to ask: what do you find relaxing or stimulating? What do you already do? Are there things you’d like to add in to your routine? What things tell your body it’s time for bed?
Ways to adapt: have your routine written down if needed and up somewhere obvious, keep what you need close to the bed; if you spend most of your day in bed, find an object, song, meditation, poem, special blanket etc. that you can associate with time to sleep and use that thing only at bedtime; do things that are relaxing for your body.
Have a hot bath 1-2 hours before bedtime as the body temperature drop afterwards will help you feel sleepy
Ways to adapt: a hot bath may be helpful for some, but may also not be possible for many. So how else could we get a drop in body temperature to help with feeling sleepy? Knowing that we need to balance this as we sleep better if we’re warm too. Could you wash your face, spend time on top of your blankets, turn down the heating for a time before bed, have a hot or cold shower, put your foot out of the blankets?
Avoid clock-watching as this can increase worry thoughts, try not to worry about having a bad sleep, rest is still good
Questions to ask: do you need a clock in your room? Do the lights of a digital clock keep you awake? Do you notice worry thoughts about not sleeping? What do you do when these thoughts come up?
Ways to adapt: notice thoughts, be mindful but try not to get caught, appreciate the rest if you can, reflect on how you feel about rest vs. sleep and how rest can still be restorative for you.
Use worry time if your thoughts are keeping you awake (worry time is a period of time set aside during the day that is purely for worrying, if you catch yourself worrying at other times notice this and put it aside for worry time)
Questions to ask: do you get kept awake by thoughts? Have you tried worry time before? Does it work for you?
Ways to adapt: set an alarm and timer, have a book and pen ready or dictate your worries to a voice recording, have a box and put worry notes away in the box, have some worry time before bed to get thoughts out of your head
Try using a sleep diary for 2 weeks to capture the facts about your sleep – this could help troubleshoot and be a good starting point
Questions to ask: what might this look like for you? What would you like to track?
Ways to adapt: ask someone to remind you to fill it in, set an alarm to fill it in in the morning, keep it next to the bed, use a template (there are lots available online), use a Fitbit or other app to help you track your sleep; it can be best to only track things for a couple of weeks to get an idea of where your sleep is at and then stop tracking in this level of detail as the over focus on time in bed and hours of sleep can increase worry about sleep, or you might choose to track in a different way after the initial period.
Exercise during the day to help with feeling tired at night, avoid vigorous exercise 4 hours before bed as this could keep you awake
Questions to ask: what kind of movement is possible for you? How long can you be active for? How can you pace out your activity so that you don’t end up overtired?
Ways to adapt: pace your day well so you’re not overtired, keep within your energy envelope, exercise may not be possible, do whatever movement is possible for you.
Food timing – avoid going to bed with a full stomach or being too hungry, big meal at least 2 hours before bed, light snack at bedtime if going to bed on an empty stomach is distracting
Questions to ask: does being hungry keep you awake? What time do you usually have dinner? Would having an earlier or later dinner suit your body? Do you have control over food timing or is someone else in charge of this? Can they help out?
Ways to adapt: have a snack available next to your bed if needed, talk to family or other supports about changing the meal time.
Sleep environment – quiet and comfortable, cool room 16-18 degrees celcius, blankets for warmth, pillows for comfort, curtains/eye mask, earplugs if necessary, take distracting things out of the bedroom (e.g. computer, TV, radio, phone, cover clocks)
Questions to ask: is your environment comfortable? Can you control the light, temperature and noise? What light, temperature and noise suit you? What’s your mattress like? Do you need a specialised bed or positioning system?
Ways to adapt: try the above, additional pillows may be needed to support positioning and comfort, may need a special mattress, have a fan with a remote; leave necessary things in the bedroom as this may be where you spend a lot of your time and removing distracting things may not be possible; some people need noise to sleep instead of a quiet environment, do you need a white noise machine, a fan or music on to help you sleep?
Consistency of daytime routine – keep daytime activities consistent, even if you’ve had a bad night of sleep, avoiding activities when you feel tired can reinforce insomnia
Questions to ask: can you still do what you had planned or do you need to adjust? Have you paced out your week/month to space out the more draining activities?
Ways to adapt: listen to your body and adjust activities accordingly, some days certain things are just not possible and that’s ok, if you need to cancel something then cancel.
See your GP if you’ve tried everything and sleep is not improving (this could be to discuss medication or a referral to a sleep specialist)
Questions to ask: have you had medical trauma? Is the GP helpful? Have you found medications helpful before? Have you already been through the sleep clinic process? Have supplements been useful? Are you actually already doing everything you can? What would it be like to drop some expectations and pressure?
Ways to adapt: take a support person, take evidence about the rates of sleep disorders in ME/CFS with you to the GP; see a different health professional, for example an occupational therapist, to help you with troubleshooting your sleep hygiene, or a naturopath to work out some supplements that might help; if there is an underlying sleep disorder, it’s important to get this checked out properly.
———————————————-
If you are already doing all you can then acknowledge this, you are trying so hard and actually doing well even if it doesn’t feel like it. All the strategies you are using will be doing something and maybe there isn’t more that you can DO. Maybe you need to let go of doing for a bit and try and find some self-compassion and take the focus and pressure off sleep. Unrefreshing sleep is tough, you don’t need to add to this by being overly critical and harsh with yourself for not sleeping in the ‘expected’ way or needing different supports and strategies to get the sleep/rest you do get.
Image description: a graphic on a tan background with blue text boxes. Heading: ‘Sleep and ME/CFS’. Unrefreshing sleep is one of the core symptoms of ME/CFS and can be one of the most frustrating. You will need to adapt and individualise the standard sleep hygiene recommendations to fit your situation. An occupational therapist is well-suited to help with this. Sometimes you can be doing all the right things and sleep is still an issue. You may need to explore whether there is an underlying sleep disorder with a sleep specialist. You may already be doing all you can. Acknowledge this. All the strategies you are using will be doing something and maybe there isn’t more that you can DO. Maybe you need to let go of doing for a bit and take the focus and pressure off sleep. Images: next to first point a person resting their head on the hand looking tired and sad; next to second point: a pencil, notebook and lightbulb; next to third point: a person in bed, stethoscope next to it; next to fourth point: a hand with a heart above it.
——————————————
I’ve also been thinking a lot about the focus on sleep and whether we sometimes over-prioritise actual time spent asleep. There are many ways to rest, that don’t involve actual sleep and this rest can also be restorative for our brains and bodies – but that may be a topic for another time!
Editing to add a bit more personalised information. I really struggle with unrefreshing sleep personally and find it incredibly frustrating. I have done a lot of work on trying to let this frustration go, appreciating rest and not getting upset on evenings when it sometimes take 2 hours to fall asleep. My brain is very busy at night and I fall asleep listening to audiobooks so that I don’t have to listen to my thoughts. Some evenings I stay up later as at some points during the month I am more alert in the evenings and I am learning to listen to and follow my body. I also know I do better when I can sleep in until 8 and generally take a couple of hours to get moving. This isn’t always possible with work hours so I do my best within the constraints of what’s going on in my life.
Picture of my bed nest. Memory foam corner pillow, additional pillows for between or under knees, weighted blanket and weighted toy to help with regulation and grounding, bamboo sheets to help with temperature regulation. I go to sleep with an audiobook on and have blockout curtains on the windows. We keep the window open so the room is cool.
I am all about individualisation and personalisation of strategies, doing what works for you and getting out of the ‘shoulds’ trap. The standard advice doesn’t take into account differences in sensory processing, pain levels, fatigue, economic or social resources and so many other things.
You know your system best so do what works for you. Create your nest, your routines and work out what strategies will support you. Additional supports from health professionals may be useful if that’s what you want to do.
[Note: the contents of this blog is general in nature and is not medical or therapy advice. If you need further support with sleep, please contact your own health professionals.]